Two considerations for regenerative medicine medical device design
I suggest that Regenerative Medicine will be associated with a parallel revolution in medicine- much like introduction of the world wide web and the internet in the ’90s caused a revolution in global communications and information technologies. As with all revolutions, history records that there are those that can thrive, adapt and ride the tides of change, and those that do not. I prefer to ride the wave.
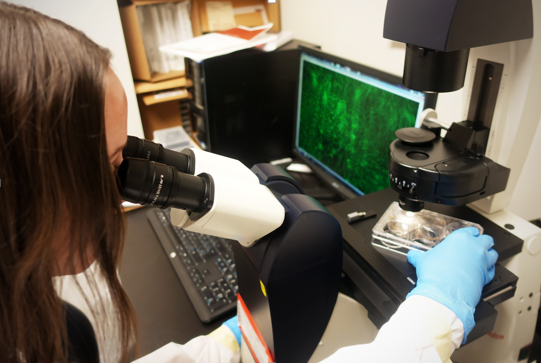
Regenerative Medicine is a rapidly growing branch of translational research where engineered tissues and cell therapies are replacing conventional pharmaceuticals, interventions and medical devices to treat disorders and restore normal function.
With that, I offer two things to consider in order to be successful developing a medical device in regenerative medicine.
#1 Do you smell a RAT?
RAT stands for the FDA’s recently put forth first interpretation of the Regenerative Advanced Therapy (“RAT”) designation program, which was established by section 3033 of the 21st Century Cures Act. The guidance can be found on the FDA’s website HERE and consists of a few short paragraphs:
- The drug is a regenerative medicine therapy, which is defined as a cell therapy, therapeutic tissue engineering product, human cell and tissue product, or any combination product using such therapies or products, except for those regulated solely under Section 361 of the Public Health Service Act and part 1271 of Title 21, Code of Federal Regulations;
- The drug is intended to treat, modify, reverse, or cure a serious or life-threatening disease or condition; and
- Preliminary clinical evidence indicates that the drug has the potential to address unmet medical needs for such disease or condition
The FDA website points readers to the Guidance for industry expedited programs for serious conditions -drugs and biologics which can be found in its entirety HERE.
In 2018, Center for Biologics Evaluation and Research (CBER) received 47 RAT requests, 16 were granted, 25 were denied and 2 were withdrawn. While comparatively low overall, RAT requests were up 37% from 2017 (the year the program was introduced). Clearly a growing field.
My point is that as regenerative medicine therapies, medical devices (in the case of engineered tissues) and related medical devices evolve, so too will the regulatory frame work and pathways. We can be sure to see regenerative and advance therapies move away from the expedited programs path to their own framework. As with traditional medical devices, always consider the regulatory path first.
#2 Good Manufacturing Practices (GMP).
GMP stands for “Good Manufacturing Practice”. GMP is quality assurance jargon for ‘document what you do’ and ‘do what you say’. As the name suggests, it applies to a wide range of industries from automotive, to food to medicine. As the regenerative medicine revolution moves from the research bench top to main stream medicine, the way in which the biological materials are made will now fall under the scrutiny of regulators. It will be required to be manufactured under GMP conditions, as would be expected for traditional medical devices or therapies.
For those of us who have worked with cell culture, you understand the very nature of growing specific cells makes the prospect of growing under standardized conditions a daunting endeavor. At the core, in vitro culture requires a substrate for the cells to grow on and nutrients to consume. Classic immortal cell lines like HeLa cells, grow well in very basic medium containing vitamins, minerals and serum.
Contrast this with Stem cells which (like the organisms they are derived from) have much more specific needs often requiring complex and varied media and substrate combinations that are finely tuned and specific to their needs. Identifying the specific combinations of growth factors, cytokines and growth combinations requires considerable effort and often leads to non-standard ‘homebrew’ growth media recipes. Further, the continual monitoring required to keep the stem cells healthy and viable tends to lead to non-standard or difficult to reproduce operating procedures.
One of the biggest hurdles in culturing stem cells in the lab is the media and procedural variability. In standard research labs, this occurs with every batch of media made (due to the person making the media, the raw ingredients, the mixing etc.). Media errors can be removed by using defined, commercially produced medium with quality assurance/quality control criteria set by the manufacturer. This provides much higher consistency in the final product from batch to batch. The result is a media with almost no variability, which improves reproducibility and efficiency of experiments across the board. Additionally, selecting media that utilizes animal-component free ingredients may be an important consideration to avoid downstream regulatory hurdles.
Detractors of GMP criticise the extremely high costs of establishing and maintaining a GMP system. The key to GMP is that it is not designed to make manufacturing more costly or time consuming, but rather to ensure that procedures are well defined and precisely followed. Application of GMP to cell manufacturing serves to generate more consistent and reproducible regenerative medicine therapies in line with conventional drugs and medical devices which are ultimately safer for the patient.
At the heart of the high-tech regenerative medicine is engineered tissues and cell therapies which are basically comprised of living cells or other fragile biological compounds. They cannot be standardised in the same way as a conventional drug or medical device.
My point is that the stem cells themselves, by the simple fact they are living cells, input a certain degree of variability in production. Understand this and strive to optimize standard protocols for cell culture conditions, selection, and differentiation techniques using well defined GMP-grade media, reagents and single-use bioprocess engineering when considering Regenerative Medicine Medical Device Design.
Nick Allan is the StarFish Medical Biotech Manager. He applies creative thinking and innovation to biomedical project commercialization from product definition through sustaining engineering.
Images: StarFish Medical
