Interference Testing, Strategy, and Detection Case Study
The importance of performing assay verification BEFORE incorporation into a medical device can not be overstated. Countless hours and dollars can be wasted designing the perfect device if the detection assay fails in the field.
Successful Point-of-Care (POC) medical devices increasingly rely on new and innovative analyte detection systems. Rapid test results, faster disease assessment and reduced health infrastructure costs have led to an explosion of assay development.
To safeguard the public against faulty designs, rigorous verification testing is required to ensure that all devices live up to their claims.
Novel assays will differ from the gold standard assays used in the clinical diagnostic laboratories. They may leverage various new and/or improved design changes, for example, in chemistry makeup, analyte processing systems, detection equipment and data processing tools. This raises the question of how to tell if your assay works as intended when there is no predicate to measure its abilities against.
To unify assay assessment between industry and clinics, guidelines have been created by the Clinical and Laboratory Standards Institute (CLSI). In this article, I will examine the assay verification guideline CLSI EP07-A2 Interference Testing In Clinical Chemistry; Approved Guideline.
What is Interference Testing?
CLSI EP07-A2 Interference Testing[1] offers methodologies and guidance to assist in determining what chemicals found in a patient sample interfere in a detection assay. This detection assay may be chemical, electrical, photometric, or others.
In practical terms, the principles of CLSI EP07-A2 ensure that investigators understand how the complex matrix of a biological sample interacts with the assay. The objective is to determine what constituents may lead to inaccurate analyte detection. Such inaccuracies can ultimately result in erroneous disease diagnoses and treatment. However, if the interferents are understood, mitigations or limits can be incorporated into sample management and device labeling.
Interferents can come from a variety potential of sources. Common sources are as follows:
- Materials taken in via ingestion, inhalation, or injection. These include foods, medications, intoxicants, or their metabolic breakdown products.
- Materials introduced during patient care e.g., pain killers, anti-clotting meds, anesthetics, and radioisotopes.
- Breakdown products from specific disease states such as cancer, diabetes, or hepatitis.
- Reagents added (intentionally or unintentionally) when collecting patient samples. Common additives include anti-coagulants, analyte stabilizers, and leachates from collection lines (e.g., vacutainer tubes, lids).
- Contaminants via poor sample handling such as touch-transfer of hand soap, cream, sanitizer, and powder from gloves.
Interferents can result in the underestimation or overestimation of a target analyte in different ways. The nature of these actions may be:
- Chemical: Chemicals may compete with assay reagents or analytes or may cause them to precipitate.
- Physical: Changes such as turbidity, surface tension or viscosity can interfere with the operation of an assay’s detection mechanism.
- Detection-dependant: This occurs when signals generated by the interferent cannot be distinguished from those produced by the target analyte – either due to chemical behaviour similarities, or the nature of the detection equipment itself.
- Enzyme inhibition: Some interferents bind or sequester critical molecules required during enzyme-based assays, thus short-circuiting the detection system.
The approach to screening potential interferents includes research, followed by bench testing. Common interferents and their concentration ranges can be found in literature. Be cautious though; these ranges will be assay- (and often equipment-) dependent.
Verification Strategy:
For efficient testing, an interference screen is performed using a technique called paired-difference testing. Potential interferents (test materials) are added to a sample pool. Assay signals are then compared to that of the same sample that lacks the test material.
In a properly designed and executed experiment, replicates of different test materials and concentrations can be screened simultaneously. CLSI EP07-A2 provides statistical guidance in designing, analyzing, and interpreting the resultant data.
Detection Case Study:
Let’s look at how CLSI EP07-A2 can be employed using a gastrointestinal (GI) POC assay utilized to detect a specific marker for Irritable Bowel Syndrome (IBS).
Scenario:
A POC medical device utilizes a chemical assay that detects a specific IBS biomarker in a patient’s GI sample. The specific biomarker causes a change in assay chemistry that can then be detected by the POC device. The assay detects the analyte in a concentration dependant manner – i.e., the more analyte– the more the change in chemistry. Detection equipment captures the chemical output, and an algorithm determines whether the quantity of analyte falls into the diagnostic range for a positive result. The resultant readout aids the gastroenterologist to assign a treatment strategy for the afflicted patient.
Interferent Identification:
Intestinal fluid (IF) is a unique environment. It is anaerobic, pH 7 – 8, and contains bile salts, mucin, enzymes, and metabolites. The environment changes with what and when the food has been ingested.
Patients with GI distress usually take medications to ease their suffering. These medications (and their metabolites) will likely be present in the IF.
However, patients may have additional underlying health concerns. Their IF may additionally contain blood, hemolytic compounds, fats and/or cancer cells.
In the above scenario, pH, bile, enzymes, bacteria, yeast, blood/metabolites, fats, and cancer cells are all potential sources of interferents in the IBS biomarker detection assay.
Interference Screening:
In the above scenario, two groups of interferents are identified. The first group are classified as physiological interferents. It includes pH, bile, mucin, blood, heme, triglycerides, yeast, and cancer cells.
The second group is classified as pharmaceutical interferents. This group investigates some of the medications expected within the GI samples. A small list includes Rabeprazole Sodium, Bismuth subsalicylate, Calcium Carbonate, Magnesium Carbonate Basic, Aluminum hydroxide, Magnesium hydroxide, and Barium Sulfate.
Clinically relevant interferent concentrations can be found through literature reviews and through CLSI. A well-designed screen includes replicates of test materials at high (worst case), medium and low concentrations expected to be present in the intestine. The relevant positive and negative controls are also included. Positive controls ensure the assay system is functioning correctly. Negative controls give the comparator to the test compounds in the paired-difference screening.
Below is an example of a physiological interference screening layout. This matrix can be performed in one 96-sample assay. The layout includes positive controls to ensure the assay is performing correctly. It includes negative controls or comparators in the paired-difference testing. It also includes several physiological interferents that are tested over 3 concentration ranges (high, mid, and low). All tests are performed in triplicate to inform statistical analysis of the resulting data.
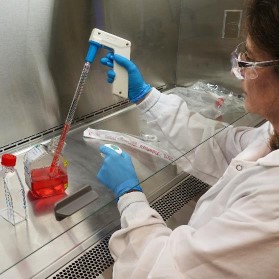
Careful consideration must be given to selecting the test fluid utilized to perform the screen. This is the sample matrix in which the test materials and controls are comprised of. Often, this fluid will be the same as the patient sample (e.g., blood, serum). However, validated simulated fluids may be substituted in initial screens when the target fluid is difficult to obtain (e.g., GI fluid, cerebral spinal fluid), or a reduction of biohazard risks is desired.
A final screen will need to be conducted in the relevant patient fluid. CLSI EP07-A2 guides the proper selection of patient test specimens and relevant control samples so that meaningful data can be extracted.
Summary
Interference screens can quickly verify if a detection assay will function in the patient test sample. It is far less costly to understand this early in the life of a medical device – before the assay becomes integrated and the system designs are fortified. Usually, assay verification happens hand-in-hand with device engineering. This allows for the design to change as required, while ensuring that all regulatory milestones are reached.
[1] Clinical and Laboratory Standards Institute. Interference Testing in Clinical Chemistry; Approved Guideline—Second Edition. CLSI document EP7-A2 [ISBN 1-56238-584-4]. Clinical and Laboratory Standards Institute, 940 West Valley Road, Suite 1400, Wayne, Pennsylvania 19087-1898 USA, 2005.
Image: StarFish Medical
Sue Bantroch is a Lab Technician at StarFish Medical. She works on a variety of biotech medical projects splitting her time fluidly between our main facility and our BSL2 facilities at the University of Victoria.