Choosing a Drug Delivery System Imaging Technology
Accurate and precise delivery of pharmaceuticals or therapies often depends on real-time imaging systems. These drug delivery system imaging techniques enhance both accuracy and precision; however, the choice of imaging method and required equipment introduces constraints that affect the design, form, and function of drug delivery systems. A thorough understanding of these limitations is particularly critical when developing a custom novel drug delivery system.
In this blog, we explore three key imaging technologies—Magnetic Resonance Imaging (MRI), Computed Tomography (CT), and Ultrasound—highlighting their advantages and disadvantages in guiding drug delivery, the constraints they impose on drug delivery systems, and their specific applications in image-guided drug delivery in the medical field.
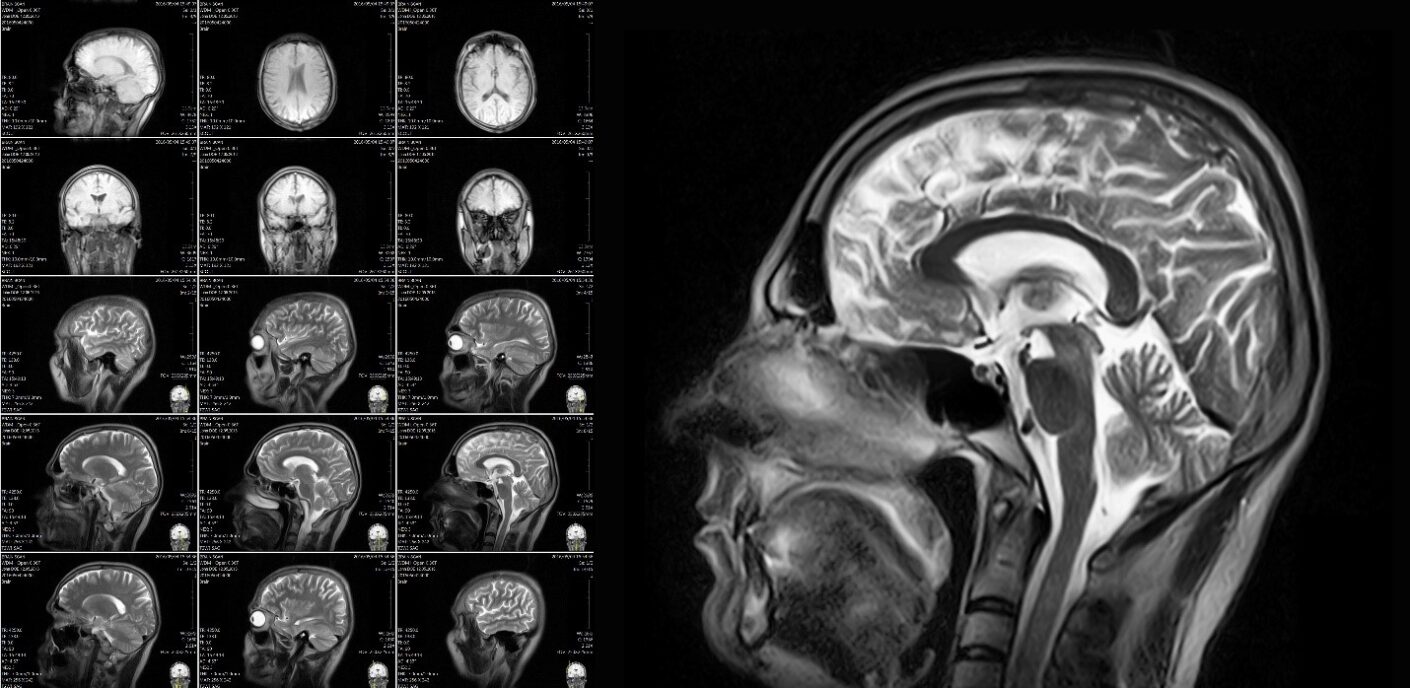
Drug Delivery System Imaging: Magnetic Resonance Imaging (MRI)
MRI is a powerful imaging technique that produces high-resolution, three-dimensional images without the use of ionizing radiation. It offers exceptional soft tissue contrast, making it invaluable for diagnosing and monitoring conditions in the brain, spine, joints, and other soft tissues. MRI’s capabilities can be extended to Functional MRI (fMRI), which assesses metabolic changes and brain activity, enabling the precise delivery of drugs for neurological conditions. When drugs are linked to MRI-visible agents, such as magnetic nanoparticles, MRI can track drug distribution and monitor controlled release mechanisms, providing real-time feedback on accuracy and drug delivery in targeted tissues.
While MRI excels at imaging soft tissues, it is less effective for visualizing bones or air-filled and fluid-filled organs, such as the lungs or gastrointestinal tract. Additionally, MRI is incompatible with certain metallic implants or devices (e.g., pacemakers, cochlear implants) unless they are MRI-compatible.
The use of MRI in drug delivery procedures introduces several constraints. Drug delivery devices must be MRI-compatible to prevent interference and ensure patient safety, requiring the use of non-ferromagnetic materials such as compatible needles and catheters. The design of these devices must account for the magnetic field and radiofrequency pulses involved in MRI.
Furthermore, MRI systems are expensive to purchase and maintain, limiting their availability, particularly for drug delivery procedures requiring intra-operative MRI suites. MRI scans also take longer than other imaging modalities, posing a challenge for time-sensitive procedures.
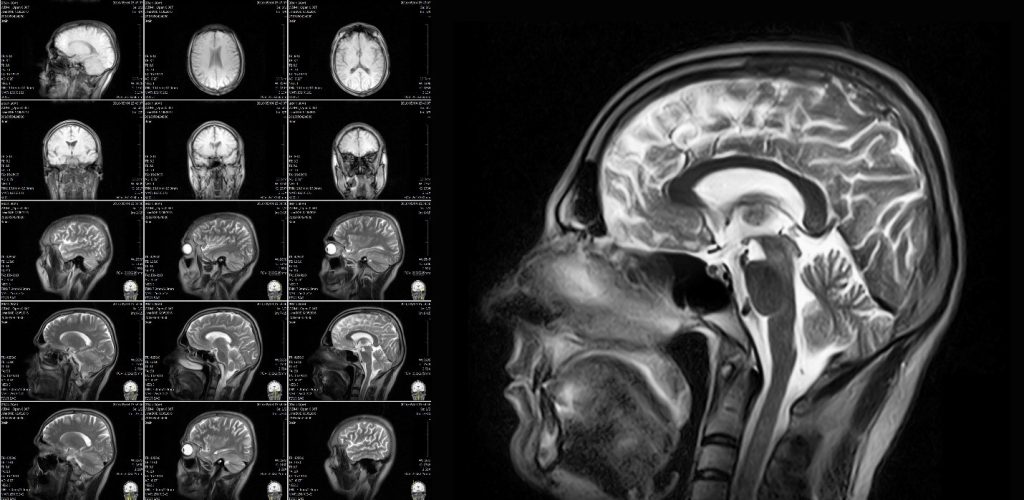
Despite the higher costs and limited availability, MRI remains critical when high-resolution imaging or fMRI is required for effective therapy delivery. A notable example of a drug delivery device is the ClearPoint Neuro Navigation System, which uses real-time MRI guidance for precise catheter placement in the brain, enabling targeted drug delivery in the treatment of Parkinson’s disease. Especially in these instances, in which MRI is absolutely required, it is favorable to design systems and processes that minimize the time spent inside the MRI scanner by shifting parts of the drug administration process outside of the MRI environment. This helps improve accessibility to the procedure and helps more patients gain access to these treatments.
Drug Delivery System Imaging: Computed Tomography (CT)
CT provides rapid, high-resolution images of various body structures, including bones, blood vessels, and soft tissues. Its ability to produce cross-sectional images is invaluable in emergency settings and for detailed anatomical studies. CT scans are quick, making them suitable for managing trauma and monitoring dynamic processes while this imaging technology also offers excellent spatial resolution, useful for visualizing complex anatomical structures. In contrast to MRI, CT scanners are widely available in medical facilities worldwide.
A disadvantage of CT is the need for ionizing radiation. This is because CT uses X-rays, exposing patients to ionizing radiation, which can be a concern, especially with repeated scans. The imaging contrast of soft tissue visualization is also lower compared to MRI, making it less suitable for drug delivery that requires extreme precision in soft tissue locations. Finally, CT is susceptible to metal implants that can cause artifacts in CT images, complicating image interpretation.
Because of the need for ionizing radiation, drug delivery systems that are used alongside CT require careful design considerations. For example, the drug delivery device needs to facilitate a drug delivery procedure that minimizes patient exposure to radiation while ensuring precise targeting. Also, materials and parts that make up the drug delivery device must be selected to avoid artifacts and generate clear imaging.
An example that is used in hospitals today is the iSYS1 Steering Device used for CT guidance to deliver drugs to specific spinal locations, treating conditions like chronic pain and cancer.
Join over 6000 medical device professionals who receive our engineering, regulatory and commercialization insights and tips every month.
Drug Delivery System Imaging: Ultrasound
Ultrasound is a versatile imaging modality that uses sound waves to produce real-time images of tissues and organs. Its portability, safety, and cost-effectiveness make it widely used in various medical applications. Ultrasound provides immediate feedback, which is crucial for guiding procedures and real-time monitoring of drug delivery. Ultrasound does not require ionizing radiation making it safer for patients, especially during repeated use. Finally, ultrasound machines are relatively affordable and portable, allowing use in diverse settings, including bedside and remote locations.

The disadvantages of ultrasound include a limited depth of penetration. Ultrasound may struggle to image deep tissues, especially if the target is hidden behind bone or gas-filled organs. The quality of imaging is also more dependent on the skill and experience of the operator. This means that greater training or experience is required for drug delivery procedures. Finally, compared to MRI and CT, ultrasound provides lower-resolution images, which can limit its use in detailed anatomical studies.
To maximize the value of ultrasound, drug delivery systems need to be designed so that they can be precisely guided in real-time. Devices must also be compatible with the acoustic properties of ultrasound and allow for the visualization of both the device and the target tissue.
One ultrasound on-market device used for drug delivery today is the Sonimage HS1 Portable Ultrasound System for guiding injections into joints and soft tissues, ensuring accurate drug delivery for conditions like arthritis and tendonitis. Another example is the use of ultrasound imaging to guide peripheral nerve blocks.
Conclusion
MRI, CT, and Ultrasound are three suitable drug delivery system imaging technologies that enhance the precision and effectiveness of drug delivery systems. Each modality has unique advantages and disadvantages that influence the design of drug delivery systems. MRI offers high-resolution, non-ionizing imaging ideal for soft tissues but requires compatible materials. CT provides rapid, detailed anatomical images but involves ionizing radiation and potential artifacts. Ultrasound offers real-time, non-ionizing imaging that is cost-effective and portable but may struggle with deep tissue visualization and operator dependency.
As technology advances, the integration of imaging modalities with drug delivery systems will continue to evolve, improving patient outcomes and expanding the possibilities for treating various medical conditions. As developers of drug delivery systems, we see an increasingly important role for customized drug delivery solutions that support accurate and precise delivery to targeted locations in the body.
Joris van der Heijden is Bio Services Program Manager at StarFish Medical. Previously he was Director of R&D at Spartan Bioscience where he led the development of a point-of-care COVID-19 diagnostic test. Joris received his PhD in infectious diseases from UBC.
