Common Pitfalls When Ramping NPI Medical Device Manufacturing to High Volume
Many Startups & Founders underestimate the importance of ramping up NPI medical device manufacturing in a small and controlled way – sort of a slow ramp. They often overestimate how quickly they’re going to require high volume and underestimate the value of post-release design changes and the effort that will be required in early launch.
Working with a large contract manufacturer (CM) right away often seems very attractive because the cost per unit appears lower. However, CMs frequently run into grief because the design is not ready for high volume manufacturing. This can result in higher cost of goods, non-conformances, or schedule slippages. This blog covers a variety of pitfalls to avoid during the manufacturing journey from prototype to commercial success.
New products generally require significant engineering support as they transition into medical device manufacturing. Managing early launch activities is challenge enough without the significant design changes that occur when you attempt to transfer an immature design into manufacture. Once the device design is in a great state, then it can be transferred to a big CM.
The less effort put into DFM (design for manufacture), the more changes will be required post-launch to solve a variety of issues. Adding cost and time to any change is the need for it to be reviewed for regulatory impact.
The above is even more applicable when a device is still in development and smaller runs are required for clinical trials or other test programs requiring larger sample sizes.
A design partner with in-house manufacturing enables efficient change control and having your thumb on the verification and regulatory environment surrounding your device. Being able to identify and address issues like material changes due to process changes will ensure that any required changes are done in a controlled manner, and as early as possible to limit the impact to inventory costs or schedule.
Clinical vs Commercial Manufacturing
Clinical manufacturing is not the same as manufacturing an approved device. The focus is on proving and refining the device efficacy and usability.
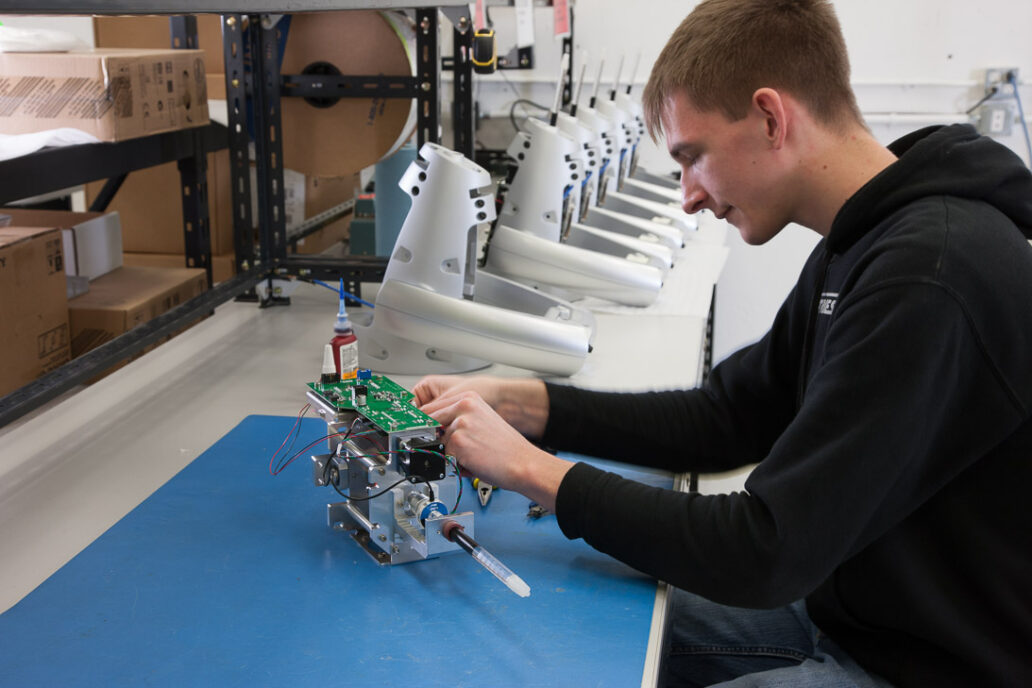
Producing product that can be used for clinical purposes is critical at that early development stage when you haven’t quite finalized the design, but implemented the core device functionality. A small number of devices must be built in order to generate clinical trial data that can support the ongoing development. These devices will be “hand made” and use prototype manufacturing methods that are a long way from the commercial manufacturing processes used to meet cost targets required for a commercial product.
Commercial products have safety and efficacy as requirements as well, but commercial devices are just that – there is a business model that needs to be met. Meeting commercial requirements are not required in a clinical trial, nor should they be – the focus is on efficacy.
There is a tendency to think that the hard part is done once a device has completed a clinical trial. And certainly that is a large part of device development. But making the 20th unit function the same as the 500th takes a considerable amount of effort, and it is often underestimated.
As a general rule, if you’ve only ever built 20 or less of these devices, you’re not quite ready to scale up to high volume. Many companies are too focused on the huge numbers they hope to sell when the product is mature.
Getting from 20 to 100 units is a big deal and to get from 100 to 200 units is a different big deal. All throughout that whole period the design is evolving as much as it did back in the prototype days. That’s when you need a partner that is really good at engineering.
Join over 6000 medical device professionals who receive our engineering, regulatory and commercialization insights and tips every month.
NPI Medical Device Manufacturing Story
It can be difficult to make one unit. Making one hundred exactly the same as that first one is an entirely different set of problems. When you build one, you are using engineering knowledge and expertise. You can make decisions as you go along to solve any issues. You’re also not noticing all of the typical production variations that you will eventually see once you order parts in quantities of in more than ten.
Everything has a tolerance. While you can make one work and tweak it, that is not a viable manufacturing process for a commercial product. That’s where NPI and commercialization comes in. It is about reducing variation so that device number 100 is just the same as the first one. And in that process learning the sensitivities of the product to those variables.
If only five or less units have been built, not all of the sensitivities will have surfaced yet. But they will appear once a bigger batch is produced. And some of the sensitivities will likely be too narrow and the device won’t work. A fundamental change may need to happen. That can be an expensive exercise to manage. When you are making hundreds of devices you will have bought tools and jigs to support large scale medical device manufacturing and these may have to be reworked.
Many changes occur after low volume manufacture – like cosmetic finish, or rebranding, or label changes. It’s often a challenge to get a desired cosmetic finish when working in really low volumes using prototyping methods as it is too early to commit to injection moulded parts.
After transition to the final design you will need to switch to a new vendor because you need a thousand units rather than ten. Such changes are often better suited for the original design/manufacturing partner and handled prior to transfer to a CM. The design partner can cope easily with that sort of change and work with your internal approval process more efficiently.
Maintaining the regulatory integrity of the device during the drive to a commercial level of consistency complicates medical device development. Managing all those little engineering changes is crucial while ramping NPI medical device manufacturing volumes up to the hundreds or thousands of units in a year. Once the device is rock solid, the above pitfalls diminish and the device can be transferred safely.
Astero StarFish is the attributed author of StarFish Medical team blogs. We value teamwork and collaborate on all of our medical device development projects.
Images: StarFish Medical