
Service Design in Medical Device Development
Designing for the Biggest Picture
Service design ensures that elements of the entire user experience are considered. From a medical device perspective, it starts from the moment a device is created to its implementation and use in a healthcare setting.
We often hear about user-centered design, which focuses on addressing the unique needs, preferences, and experiences of users. Patient-centered design, a specific type of user-centered design, develops solutions tailored to patients, but what about the clinicians and the rest of the hospital staff? Designing for these stakeholders is equally important, and this is where service design comes into play.
When designing medical devices, it is easy to think of the patient in terms of the key user, however, patient care is influenced by many individuals, such as nurses, doctors, maintenance staff, educators, following the policies that are in place. Patients’ conditions are significantly affected by the care they receive from all of these people.
Medical devices are created to improve and save lives. Failures can lead to unfortunate outcomes. Therefore, it is important to consider the perspectives of all the individuals that interact with and support the patient when developing medical devices or products in order to ensure comprehensive and effective solutions and eliminate any adverse outcomes.
What is User-Centered Design?
User-Centered Design, or UCD for short, ensures that every element of the end-to-end experience between a user and a desired/expected result or outcome is smooth and meaningful. It involves studying users’ behaviors, needs, and motivations to create products that provide impactful and relevant experiences.
In the medical field, the most common users are the clinician and the patient. However, it is important to understand that a user could refer to anyone who interacts with a device including caregivers, support staff, cleaning/sterilization staff and laboratory technicians to name a few.
User-centered design…
- Focuses on the individual user experience, primarily improving users interact with medical devices. It is concerned with specific touchpoints and ensuring that the product meets the user’s needs effectively.
- Involves user research, usability testing, and iterative design processes to develop and refine the device.
- Improves the usability and effectiveness of the device for the end user. It ensures that the device is intuitive, eliminates potential use error and meets the specific needs of the end users.
Distinguishing Service Design from User-Centered Design
You could think that Service Design is a methodology that designs for the biggest picture, like layers upon layers of user-centered design. It is highly collaborative and focuses on complex system processes, technologies, and interactions to provide holistic solutions and services to multiple stakeholders within unique contexts.
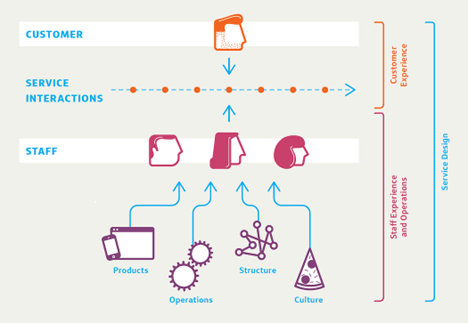
The diagram illustrates how Service Design works and how medical devices fit into the big picture. In the context of healthcare and medical devices.:
- Products: Represent the medical devices.
- Operations, Structure, and Culture: Represent the components of the healthcare system.
- Staff: Represent the healthcare employees.
- Customer Experience: Represents the patients.
- Service Interactions: Represent the interactions between staff, their products, operations, and culture, and the patients, and vice versa.
Users exist within a complex chain of interactions, not in isolation. To meet the diverse needs of different users in different contexts, it is essential to understand the relationships between those who receive and provide the service. Only then can effective devices be developed for users from different ecosystems.
In the medical device space, service design:
- takes a broader view, considering the entire healthcare ecosystem. It aims to optimize the interactions between all stakeholders involved in the healthcare process, including patients, clinicians, and support staff.
- utilizes service blueprinting, stakeholder analysis, and a holistic design approach to ensure all elements of the service (in this case, the medical device) work together seamlessly.
- enhances the overall efficiency and effectiveness of the healthcare system by ensuring that the device integrates well into the broader healthcare ecosystem (which has deep-rooted cultural and environmental complexities).
Service design involves considering all stakeholders and ensuring that all channels align seamlessly, from backstage (doctors, nurses, and staff) to front stage (patients). It’s not just the patient who uses the medical device; it also includes medical professionals, caregivers or family members managing conditions at home, telehealth providers, and other care delivery stakeholders. By addressing the needs and interactions of these diverse groups, service design creates a more integrated, efficient, and overall inclusive healthcare experience.
Role of Service Design in Medical Device Development
While service design and user-centered design both aim to improve user experiences, they are distinct in approaches within the design space. UCD ensures that medical devices meet the specific needs of those using the device (usually clinicians or patients). SD ensures the device(s) bridge any gaps and fit seamlessly into the complex healthcare system. Considering both approaches can lead to better-designed products that are not only user-friendly but also improve the efficiency and effectiveness of healthcare delivery for both patients and healthcare staff.

Including service design in medical device user-centered design
Taking a SD approach along with UCD can provide many benefits in the process of creating medical devices. They include:
- Better patient outcomes: By meeting individual needs and improving system-wide interactions, devices can provide better overall care.
- For example, developing medical devices that offer personalized treatment plans, such as customized medication dosages or therapy schedules, can improve overall care by catering to the specific needs of each patient.
- Improved employee experience: Providing healthcare professionals with the relevant tools and processes results in more efficient and satisfying work environments.
- For example, designing an intuitive, user-friendly interface for an electronic health record (EHR) system can streamline the documentation process for nurses and doctors. This reduces the time spent on administrative tasks, allowing healthcare providers to focus more on patient care, thus leading to a more satisfying and effective work environment.
- Optimized processes: A holistic approach helps reduce bottlenecks and inefficiencies in the healthcare system.
- For example, in the scenario of remote patient monitoring, creating a centralized telehealth platform that integrates with various medical devices and EHR systems can streamline the process of care between the patient and the provider. This comprehensive approach reduces bottlenecks by allowing healthcare providers to efficiently access and manage patient data, resulting in improved coordination and faster decision-making.
AI Implications (or) Some Exceptions
However, while service design offers numerous advantages, there are scenarios where its application may be limited or less impactful for certain medical devices, particularly devices that are integrated with Artificial Intelligence (AI).
The FDA has authorized 882 AI/ML-enabled medical devices as of May 2024. These authorized devices serve as assistive tools in various medical specialties including cardiology, radiology, neurology, and hematology. They are designated to work alongside healthcare professionals to provide support and improve patient outcomes.
While there aren’t (yet) AI-driven medical devices that fully operate autonomously with minimal to no human interaction, it is only a matter of time before they emerge. This is an active area of research and interest in the healthcare field. With that in mind, when developing such products, it is important to always remember why we are designing them and who will be using these devices—humans. Otherwise, we will be limiting our potential to further improve the interoperability and user experience of medical devices. It is important to tread carefully and evaluate the appropriateness of AI integration, considering the context and objectives.
While service design offers valuable improvements for many medical devices, its approach may not be necessary for some. Nevertheless, for most medical devices, especially those involving complex interactions and multiple stakeholders, service design remains a powerful approach to enhance usability, efficiency, and overall healthcare outcomes of medical devices. Ultimately, service design must be about the people, not machines.
Once again…
In the development of medical devices, it’s important to focus on both the frontstage and the backstage. Regardless of whether you’re designing a product or service, user-centered design should never be taken out of the equation because both should be designed with users in mind. By implementing service design, we can create comprehensive and holistic medical devices that address the needs of all individuals involved. This ensures that devices provide meaningful user experiences while also enhancing overall healthcare outcomes.
At StarFish Medical, service design is crucial for value creation, benefiting everyone involved – from our product development team to our clients and then their end-users.
Jersey Stuart is a Visual Designer Co-op at StarFish Medical for the 2024 summer term. They are studying Design at York University, specializing in visual communication and digital design, with a focus on advocacy and human-centered design.
Reference List:
- Key Concepts in New Service Development by Bo Edvardsson and Jan Olsson
- What is User Centered Design (UCD)? — updated 2024 | IxDF (interaction-design.org)
- SDN | What is Service Design? (service-design-network.org)
- Patient-Centered Design: Definition, Applications & Challenges (dovetail.com)
- How medical device and service designers balance form… | PA Consulting
Read our overview of the FDA action plan for AI/ML in software as a medical device with best practices.
