Medical Device Labeling Requirements: Compliance and Best Practices
We all know medical devices have labels, but how often do we consider their purpose and the effort required to ensure they provide the right information? Device labelling serves as the interface between the manufacturer, the user, and regulatory bodies. (Note that being from Canada, we spell labelling with two Ls.)
Labelling is not just about marking a product with a brand name or model number; it involves clear, accurate, and comprehensive information that complies with regulations and standards set by authorities like the FDA, Health Canada, and Competent Authorities in the EU, as well as international standards groups such as IEC (International Electrotechnical Commission), which oversees the 60601 series of technical standards for the safety and essential performance of medical electrical equipment.
This blog aims to help medical device developers understand the key factors involved in defining device labelling requirements.
Before we jump in, let’s clarify that device labelling refers to the information provided on or with a device. This can include printed labels, user manuals, graphic information (e.g., symbols), or even digital content. The primary goal is to ensure that healthcare professionals, patients or any stakeholders who handle the device are informed about its proper use and storage, safety precautions, and regulatory compliance. The following sections outline common considerations for defining labelling requirements.
The Basics – Physical Labels
Labels should always identify the device and its manufacturer. This includes the device name and model number, contents of the packaging, serial number or lot number, and for the US and EU, a Unique Device Identifier (UDI). Additionally, it must contain the name and address of the manufacturer and contact details, and, if required, information on the importer or distributor.
Dates are also key. These may include the date of manufacture, an expiration date, or a shelf-life date.
This information is typically printed on a physical label affixed to the device or its packaging. However, if the device is too small, it may be provided as a product insert.
The Basics – Accompanying Information
Commonly referred to as the “Information for Use” (IFU) and sometimes called user manuals, these are typically provided as booklets or downloadable electronic versions. The IFU is a detailed and comprehensive document that provides a description of the device and how it functions, instructions on how to set up, operate, maintain, store, and dispose of the device, as well as information on how to safely use it, including warnings and cautions to prevent hazardous situations.
One of the key elements included in an IFU is the intended use and indications for use. The former succinctly outlines the general purpose of the device, while the latter provides context such as the circumstances for use, medical condition, anatomical subject, use environment, and patient population.
Special Considerations
Devices—whether sold as sterile or requiring sterilization before use—must include specific information on their packaging and in the IFU. This includes symbology indicating sterility, whether the device can be re-used, the method of sterilization (e.g., autoclaving), storage or disposal requirements, and, if applicable, details on reprocessing.
Non-sterile, reusable devices require reprocessing or cleaning instructions. These instructions may range from simple cleaning steps before or after use to complex reprocessing protocols requiring extensive validation.
The IEC 60601 series of standards dictates specific labelling requirements for electronic devices, including both physical labels and IFU details. Additional content may include markings related to product classification, grounding instructions, isolation requirements, environmental conditions such as temperature and humidity limits, transport and storage conditions (e.g., special handling markings), technical descriptions, and patient and user protection instructions. If your device requires conformance to a particular or collateral IEC 60601 standard, additional labelling requirements may apply.
Manufacturers of in vitro diagnostic devices have a collection of symbols at their disposal to identify reagents, quantities, control material, and testing scenarios such as self-testing and near-patient testing.
Compliance Marking
In some jurisdictions, compliance labelling is required to indicate a device’s regulatory status. The EU requires a CE Mark (Conformité Européene) for devices that conform to the Medical Device and In Vitro Diagnostic Devices Regulations (MDR and IVDR, respectively).
Devices certified for electrical safety require a mark issued by the certification body upon completion. Additionally, several jurisdictions (FDA, Health Canada, EU) require statements on the device if it is being used for clinical investigations or non-human-related research.
Risk
Device complexity and safety profiles often correlate with the extent of required labelling. Although risk is linked to compliance-driven labelling requirements, the risk management process outlined in ISO 14971 often dictates much of the required labelling. This is done through the risk assessment process by defining risk control measures and residual risks that lead to information for safety. For example, many warnings and cautions communicated in the IFU result from use-related risk mitigations. Other identified hazards—mechanical, electrical, chemical, or biological in nature—may also drive IFU requirements and additional markings on the device.
Conclusion
Labelling is more than just printing basic product information on a sticker or fulfilling a compliance checkbox—it is a critical communication tool and a key component of risk mitigation.
The above is just the tip of the iceberg. Many other considerations go into labelling, such as material choice, design, and verification and validation activities. To get started, familiarize yourself with the specific requirements set by regulatory bodies and standards. Have a look at the reference list below to get started, and happy labelling!
Deborah Pinchev is StarFish Medical’s Toronto QA/RA Manager. She is inspired to write blogs by her interest in helping companies develop and bring to market new and innovative devices.
Images: Adobe Stock
References
- Code of Federal Regulations, Title 21, Part 801, Medical Device Labelling
- Code of Federal Regulations, Title 21, Part 812.5, Labelling of investigational devices
- Canada Medical Device Regulations (SOR/98-282): Part 1 Section 21 Labelling Requirements, Section 43.5 Marking and Labelling; Part 2 Section 75 Labelling, Part 3 Section 86 Labelling
- 2017/745 EN Medical Device Regulation (MDR)
- 2017/746 EN In Vitro Diagnostic Medical Devices Regulation (IVDR)
- IEC 60601-1:2005+A1:2012+A2:2020 Medical electrical equipment – Part 1: General requirements for basic safety and essential performance
- ISO 15223-1:2021 Medical devices — Symbols to be used with information to be supplied by the manufacturer — Part 1: General requirements
- IEC/TR 60878: 2015 Graphical symbols for electrical equipment in medical practice, for description of symbols.
When it comes to risk, the first thing to consider is the ISO 14971 standard. MDR and IVDR changes bring a new alignment in terms of risk.
One product standard we deal with frequently is IEC 60601-1 Medical Electrical Equipment – Part 1: General Requirements for Basic Safety and Essential Performance. Bjarne Hansen distills its essence to help readers understand where some of our design decisions come from.
Related Resources
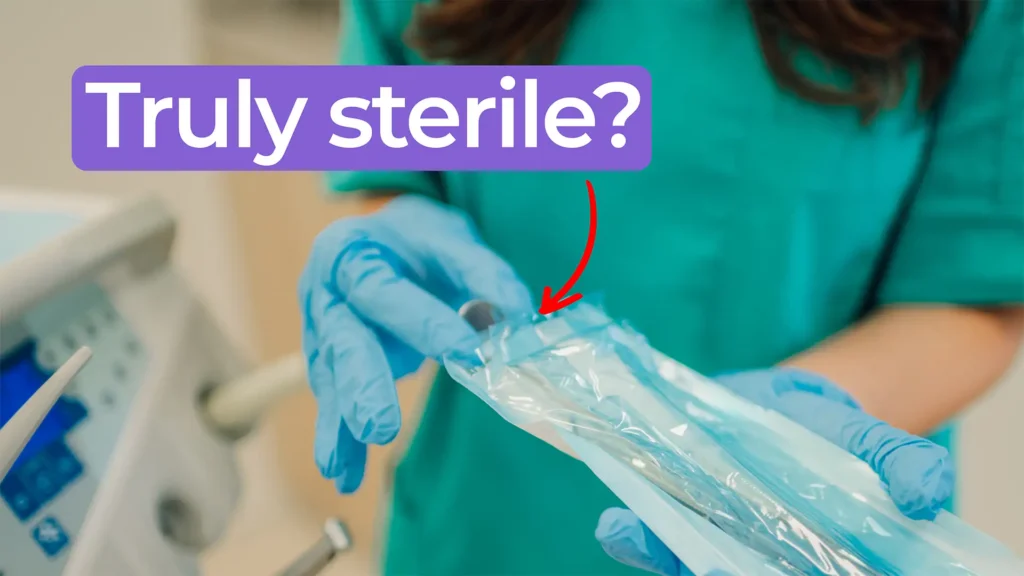
Nick and Nigel walk through how sterile disposables are processed and verified before they reach the field.
The FDA agentic AI is making headlines after the agency announced its own internal AI review tool. In this episode of MedDevice by Design, Ariana and Mark discuss what this could mean for medical device submissions and regulatory efficiency.

The sandwich ELISA assay is one of the most common ELISA formats used in diagnostics. Nick and Nigel walk through the method step by step using simple visuals and plain language.

For manufacturers of novel devices that can make a significant impact to patient health, the goal of the program is to offer a path to streamlined and potentially faster market entry without sacrificing the rigour around ensuring safety and performance.