Simulated Fluids for POCT Development
An expensive pitfall when developing or optimizing a point-of-care device is to jump straight into using clinical samples to steer early design development. Developing or optimizing a point-of-care device is a multi-faceted process.
It includes developing a test platform, reagents, device materials and potential software tools for analysis. One critical aspect of moving your concept forward is understanding the interactions that take place between your device and the sample fluid that it is designed to test.
In this article, I will explore ways in which simulated fluids for POCT developments can streamline the development process, help design to eliminate system variability, mitigate design risks, and control overhead costs.
A fundamental requirement for designing a Point of Care Testing (POCT) assay and device is that all external and internal sources of variability need to be understood. Simulated fluids (SFs) enable an investigator to tailor-make a liquid that mimics the critical properties of the desired clinical sample. The power comes from removing the inherent variability and complexity of human-derived fluids. This allows engineers to focus on inherent variability that is driven by other factors like: the equipment (device-to-device, run-to-run), reagents (different reagent builds, different suppliers of raw materials, storage conditions or shelf life), user (different operators or different days of operation) and user environments (different temperatures, different humidity, etc.).
Understanding what factors lead to different outcomes helps eliminate potential drivers of variability and helps development of appropriate software algorithms for signal analysis. Taken together, they will help engineers make sound data-driven design decisions unclouded by sample-to-sample variability.
Wisely chosen simulated fluids for POCT development can afford the design developer with the following benefits:
- Representative: A good recipe can mimic the chemistry and physical characteristics of the clinical sample. Factors such as salt balance, pH and/or viscosity (to name a few) can be changed and controlled to reflect changes in patient physiology or disease state.
- Reproducibility: Large batches of simulated fluids for POCT development can easily be made and used over many experiments. This gives an investigator the power of reproducibility during assay development. One constant formulation can be utilized to investigate numerous test reagents without introducing the variations associated with a human-derived clinical sample.
- Simple: SFs lack the complex, fluctuating components found in native fluids. It is much easier to determine cause-and-effect during assay development and optimization when using a simple fluid that you can control.
- Accessible: Many SF recipes are easily made on benchtop, requiring general laboratory skills and equipment. Many sources are also available from scientific supply companies.
- Cost-effective: Many SFs can be made or bought inexpensively – especially compared to obtaining similar volumes of the human equivalent.
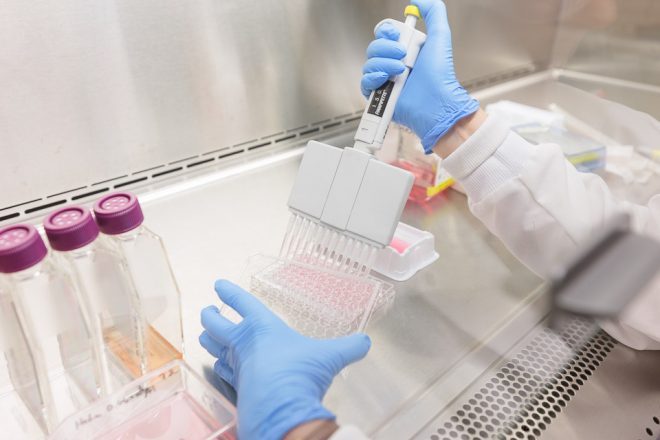
- Bio-hazard-free: Human-free ingredients can often be chosen to make a SF formulation. This mitigates the risk of acquiring deadly or debilitating diseases associated with using clinically-derived fluids. Early bench work can take place in a general chemistry or engineering lab – as opposed to in an expensive, biosafety level 2 containment facility.
Here are a couple of common scenarios which highlight benefits of using SFs in early POCT design:
Down selection of construction materials and reagents
Designing a lateral flow strip technology This strip must detect a low quantity peptide in gastric fluid that is associated with stomach cancer. Human gastric fluid is a complex liquid that varies with person, fasting state and disease state. Using a patient gastric sample in early product design will only lead to inconsistent, contradictory or inconclusive test results.
To efficiently design your POCT, you need to have full control of your testing system right from the start. This is accomplished by using a chemically defined, simulated gastric fluid (sGF). Numerous recipes and products are commercially available that mimic the basic component of gastric fluid.
Start by preparing a basic simulated gastric fluid. A simple recipe might look like the following: 2.0 g NaCL + 7.0 mL HCL per 1 L H2O; pH 1. Now, you can add (and/or vary) individual components in order to test the range of pH, viscosity, osmolality, protein and enzymes expected in your target patient population. As you systematically challenge your device or assay system with the full sGF dynamic range, look out for the following failures:
- Break down of your lateral flow material or layers
- Degradation of the antibody bound to the strip
- Interference with the labelling system
For example, a lateral flow pad that disintegrates in sGF with pH 1 will also break down in human stomach acid of the same pH. You can use this technique to quickly screen a large variety of lateral flow strip materials, and reagents until you find a suitable combination. Conversely, you may find that you need to integrate a pH neutralizer for your technology to work.
Analyte optimization
Developing a microfluidics test cartridge This cartridge should detect the presence of a viral peptide from cerebrospinal fluid (CSF). For this study, let’s look at assay development and optimization.
Human CSF is a mixture of salts, glucose and specific bio-active proteins. Generally, a sample of human CSF is acquired through a painful and risky lumbar puncture. The quantity of fluid obtained from one patient is very small. Although it can be purchased commercially, it is unsurprisingly, quite expensive.
With such constraints, it is extremely important to optimize as much of your microfluidics system as possible before attempting to assay the human version. In this case, simulated cerebrospinal fluid (sCSF) will be used to screen your test reagents.
A typical sCSF recipe might look as follows: 150 mM Na, 3.0 mM K, 1.4 mM Ca, 0.8 mM Mg, 1.0 mM P, and 155 mM Cl. This homogeneous, inexpensive reagent is ideal for screening target viral peptides/antibody combinations and concentrations, buffers, blocking agents, and detector components. You will be able to investigate lyophilized versus liquid reagents in your cartridge before finalizing hardware and software design.
Verification/Validation
Verification and validation testing is required regardless of the POCT system being developed. Prior to locking down design plans and entering into expensive clinical trials, verify the analytical performance of your system to confirm that your product can produce test results that are analogous to those obtained via accepted clinical assays and equipment. Much of this verification can be accomplished using the appropriate simulated fluid and your analyte of choice.
You need to know early on if your system can meet the sensitivity or specificity of the gold standard. Results from analytes spiked into SF will immediately tell you if the assay is working. If not, troubleshooting results from this simple configuration is definitely easier than troubleshooting results from inherently variable clinical samples. At this stage, clinical samples will only add complicating questions such as:
- Did the clinical sample contain the analyte of choice?
- Was the sample obtained and handled properly before you received it?
- Did the patient take medications that are interfering with your test?
- Was the sample stored and handled exactly the same before being used on your system versus the conventional test to which you are comparing it to?
Now that you have confidence that the assay can detect your analyte in the “best case scenario”, you must also have confidence that it can detect it under less than optimal circumstances. Human clinical samples from both healthy and diseased patients may contain contaminating or interfering substances.
Common materials to look at may include whole or hemolysed blood, carbohydrates, bio-active proteins, medications or metabolites. These substances will be specific to the type of body fluid being tested and the types of diseases that your patient population may be experiencing. Start validating the early stage assay by testing matrices of interfering compounds against your analyte/SF combo. This information will draw attention to any deficiencies that need to be addressed before handling the complicated clinical fluids.
Upon completion of this testing, you will have confidence in the robustness of the system. If the assay is generating accurate, reproducible results that are comparable to the industry standard, it is time to move forward with analogous tests using your target human fluid.
Even if you are converting a standard benchtop procedure to a cartridge-based assay, you will need to follow these same assay development and optimization principles.
A word of caution…
There is one important note I would like to make about choosing the right simulated fluid recipe for developing your assay. Perform your due diligence!! There are many recipes available for virtually any simulated fluid. However, remember that these fluids have been developed to perform specific functions which may directly conflict with your assay.
Research and understand the purpose of each ingredient in your SF recipe before incorporating it into your testing regimen. For example, consider a POCT assay to determine the presence of a virus in sputum samples by using an antibody detection system. You have found a simulated sputum recipe that contains egg yolk – a complex ingredient not found in natural sputum. You further find that it is used as a viscosity enhancer when testing biofilm formation of Pseudomonas aeruginosa bacteria in a cystic fibrosis lung models.
Before using this recipe, determine whether egg yolk will have any deleterious effects on your assay system. Will it mask viral antigens? Will it bind to or degrade antibodies? Will it quench signal detection?
Another consideration is the storage conditions and shelf life of your SF. To reduce batch-to-batch variability, it is desirable to prepare a larger batch all at once and store smaller aliquots of the SF to be taken out of storage immediately prior to experiments. Understanding the effect of storage and freeze/thaw cycles on the stability of your SF helps experimental planning and reduces variability driven by batch-to-batch variability of your SF. Make sure that the recipe and the way you store the SF will answer your questions clearly – and not muddy the waters even further!
Ready to go!
With this knowledge, you can optimize simulated fluids for POCT Development that will become crucial to your testing program. Understanding your assay and equipment will help you understand your SF requirements. Understanding your SF components will help you understand your assay and equipment performance and limitations. Go and make a great device!
Sue Bantroch is a Biomedical Engineering Technician at StarFish Medical. She works on a variety of biotech medical projects splitting her time fluidly between our main facility and our BSL2 facilities at the University of Victoria.
Images: StarFish Medical
