Top 10 COVID-19 Medical innovations
Rapid technological advancement is often triggered by external events such as international conflicts, political pressure, economic downturn, competitions or disease. COVID-19 Medical innovations fall into this category.
The COVID-19 pandemic has triggered the drive for technological advancement. Scientists, engineers and innovators have risen to the challenge by doing that which they do best – designing, building and prototyping.
Here are my top 10 COVID-19 medical innovations.
#10 COVID-19 Medical innovations: Robotics
Robotic technologies are of the top 10 COVID-19 Medical innovations and have been utilized in many ways during the current pandemic: Robots were designed to communicate between patients and doctors at a distance (a); to disinfect surfaces with UV light (b) ; to deliver essential medical supplies; to monitor vital signs (c) ; to remind people of infection prevention measures like social distancing; and to scale-up production of diagnostic tools, drugs and vaccines.

It’s heartwarming to hear that robots lighten the workload of health care providers and help them keep their distance from infected patients. Delivery robots bring food and supplies to homes of at-risk people protecting them from delivery workers potentially infecting them. Social robots interact with patients in quarantine to keep them company in the absence of human visitors.
Telepresence robots are deployed in nursing homes to help family members connect with isolated elders via social media platforms. There are many innovations involving robots performing telemedicine. Robots could also be designed to give patients high-quality emergency consultations for stroke, cardiovascular, and burn injuries. During the COVID-19 recovery period, they could monitor patients and serve as a direct link to medical professionals in the hospital or even at home.
#9 Drones
Canada-based drone (a) tech firm Draganfly is rolling out stationary cameras and drones to detect people with COVID-19 symptoms. Drone engineers and enthusiasts use drones to monitor social distancing measures in a large gathering (b) and to deliver essential medical supplies to remote hospitals and clinics. Virus spotting drones (c) were also used as early diagnostic tools by obtaining people’s temperatures and identifying the possible spread of infection.
Engineers equipped drones with speakers to remind people of quarantine protocols. Even though drones are not considered medical devices based on their intended use, their role as support tools should be recognized in our health care system.

#8 UV-C Disinfection
Sanitation and disinfection are a primary tool in our healthcare system to prevent the spread of infection. People want to be sure that their place of work and anything they will touch is safe and free from the virus. In hospital settings, it is crucial that operating rooms or ICUs are routinely disinfected and sanitized. Any human or procedural error during the disinfection can cause hospital-acquired infections (HAIs).
Studies shows that HAIs cause patient mortality or illness, longer hospital stays, and additional cost of services just to contain infections, among other issues. The most commonly used disinfection tools are liquid and sprayed disinfectants, which can be complicated and burdensome to use effectively. Product development engineers are exploring a new approach using ultraviolet lights in the so-called UV-C range (100-280 nm). Applications include ICU and patient room disinfection (a), sanitizing gadgets such as mobile phones (b), personal devices, air purifiers, and N95 masks for possible reuse (c).
This technique does not require liquid disinfectant, but rather disinfects by exposing the affected area to UV light. Research papers have demonstrated that UV light at the proper intensity and duration can kill 99.9% of bacteria, fungi and viruses. There are also new product concepts for sanitizing individual work stations and conference rooms with UV lights on a regular basis.

#7 Vital signs monitor
It is mandatory to monitor COVID-19 patient vital signs during illness as well as during the recovery stage. Vital sign monitors constantly check blood oxygen saturation, heart condition, breathing and the movement of the patient. Since COVID-19 targets the lungs, it is obligatory to monitor the blood oxygen saturation (SpO2) also known as “peripheral capillary oxygen saturation”. SpO2 refers to the percentage of red blood cells that are saturated with oxygen. As per interim guidance from World Health Organization (WHO), in a young adult severe pneumonia accompanied by high fever or a respiratory anomaly and a SpO2 level of less than or equal to 93% is one of the major symptoms of COVID-19. A normal healthy person should be able to achieve SpO2 levels of 94% to 99%. For patients with mild respiratory diseases, the SpO2 should be 90% or above.

In my opinion, to effectively monitor patient vital signs, the sensor should be wearable. It could be a device worn on the wrist, a necklace, an attachment to the body (c) or even as head gear, as long as it does not affect the mobility of the patient and can be comfortably worn for a long period of time.
While in quarantine at home or recovering from the disease, wearable vital sign sensors provide peace of mind and assurance about a person’s health. Some companies have launched wearable vital sensors, some are still in the development stage, and others are in clinical testing. Examples include a wrist band for SpO2 monitoring(a), a sensor for monitoring breathing and body temperature(b) and a biometric sensor with location and position tracking(c).
#6 PPE
Medical practitioners must protect themselves from infection using personal protective equipment (PPE) such as face shield, gowns, gloves and masks. However, due to the huge inflow of COVID-19 infected patients to the hospital and clinics, the supply of required PPE was initially insufficient. A number of medical personnel became infected and died after helping patients as a result of limited PPE, lack of proper training, and monitoring of use. With the shortage, the government requested that the private sector and suppliers produce more.

Personal protective devices such as protective clothing was designed and made using surgical drapes and plastics (a). Diagnostic testing booths equipped with HEPA filters (b) were made to reduce the use of surgical gowns and medical supplies. This booth is more comfortable for healthcare personnel and lowers the probability of infection during the removal of gowns. Lots of innovative solutions for face shields were developed (c). These range from face shields made using 3D-printed frames and thin plastic binder sleeves, to fashionable consumer face shields. Recent research casts doubt regarding the efficacy.
#5 Portable dialysis machine
News reports indicate more COVID-19 patients in ICUs need dialysis. Emergency room doctors reiterate they are running into a shortage of dialysis machines and supplies. Aside from kidney failure, the patient’s intense reaction to the virus often causes blood to clot. These blood clots literally clog the dialysis filters and these filters are in limited supply. This is a huge challenge.
Dialysis machines are usually situated at clinics where patients go regularly. However, with social distancing and COVID-19 patients requiring such a procedure, a new treatment methodology has evolved. The patient has the option go to the dialysis center or to use a benchtop or portable dialysis machine that can be operated at the doctor’s office or even at home.

Companies in Europe have designed and promoted dialysis machines for home use. In this home use model, nurses will go to each home by appointment to administer the dialysis procedure. Others designed a wearable model (a) that could be attached to the body as the procedure is being done. StarFish Medical worked on the early designs of the HD+ home dialysis system, which is now Tablo from Outset Medical and was cleared by the FDA in April 2020. There are benchtop (b) and portable models (c) that are currently being developed. Most of the wearable and home use dialysis machines are not yet approved by the FDA and therefore, not yet available in North America.
# 4 Telemedicine and remote monitor
In the absence of a vaccine, activities such as meeting people, gathering with a crowd and even visiting a doctor are a challenge. Innovation in communication using teleconferences or online consultations has increased significantly. Telemedicine was promoted several years ago, but gained little traction. However, during the COVID-19 pandemic, telemedicine now delivers medical care remotely to millions using communications technology(a). By using more sophisticated technologies like videoconferencing and other new emerging applications, telemedicine will continue to become popular in our health care system.
Innovation for a customized application platform that has the ability to securely share and store sensitive health data is in high demand. A telemedicine platform must meet the requirements of the Health Insurance Portability and Accountability Act (HIPAA) and be capable of capturing data sent from diagnostic (b) or vital sign monitoring devices (c) at the point of care. Emerging telemedicine platforms include connected devices such as heart monitors, SpO2 sensors, blood pressure monitors, digital stethoscopes and other home diagnostic equipment.

#3 Ventilator
The COVID-19 fatality rate is estimated to be 3% of the infected cases. The SARS-CoV-2 virus causes respiratory disease and affects cells in the nasal cavity, bronchia and lung. In severe cases, the patient may experience significant difficulty breathing requiring a ventilator intubated into the lungs to support breathing. Usually, intubated patients stay on the ventilator for days and even weeks. With the limited availability of ventilators in the health care system, many patients can’t survive.
In North America and Europe, the need for the ventilators was publicly announced. In Canada, several local companies were awarded contracts by the Federal government to produce 40,000 units in anticipation of the country’s ventilator requirements. They include Thornhill Medical (a), CAE (b), Ventilators for Canadians and a group led by StarFish Medical(c) to produce up to 30,000 ventilators.

#2 Face Masks
With the shortage of masks for healthcare workers and increasing global interest in protective masks, innovative ideas have come to light.
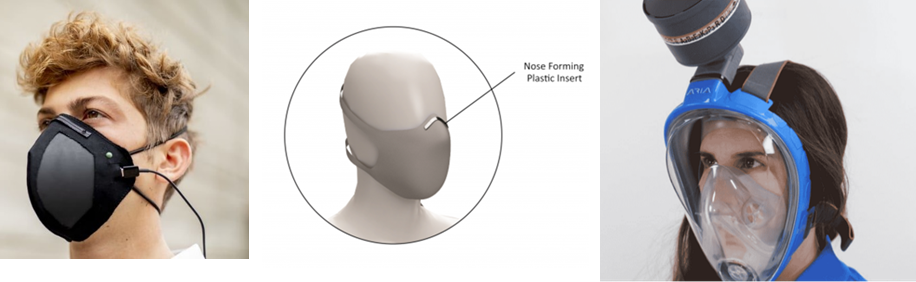
One high-tech mask is the ‘Guardian G-Volt’ breathing mask (a). It utilizes a laser-induced Graphene filter that works to trap and even repel viruses, bacteria and a range of other pollutants. It uses a low-level charge that is delivered to the unit via USB and enables it to be 99% effective at blocking particles larger than 0.3 microns. Another innovative mask is designed for the dental industry. Dental health care providers are considered the most vulnerable medical sector for infection. Myant, a Canadian company, announced that they developed a mask (b) for dental professionals. Their masks include a washable textile and textile-based respirators.
How about a full-face snorkeling mask with a filter attached? Snorkel gear(c) was repurposed as a mask to serve as protection against infection. This device was made by an Italian company, Mestel Safety, part of the Ocean Reef Group. There are a number of other companies that design and prototype different interesting masks for medical and consumer use. The use of face masks is here to stay until a COVID-19 vaccine becomes available to public.
#1 COVID-19 Medical innovations: COVID 19 Diagnostic kit at Point of Care
Diagnostic tools for detecting COVID-19 are on the top of my list. In any communicable infection scenario, the most important aspect is to detect who is and who is not infected with the infectious agent as quickly as possible. For COVID-19, it is difficult to detect the level of infection because of its unique way of infecting people. According to the CDC, the first 1-5 days tends to be asymptomatic. This means that the infected individual does not manifest any symptoms even though the individual is already infected and does not know that they may have started to spread the disease. After that stage, the person starts to show symptoms and the disease antibodies start to be detectable. The most common symptoms are fever, body aches, difficulty of breathing, and loss of smell among others.
To identify and track all infected individuals, it is of prime importance to test practically everybody.
Some companies have repurposed their existing platforms and adapted them to detect SARS-CoV-2 RNA. Taking into account that this disease can be asymptomatic, the most accurate tools will be nucleic acid tests (RT-qPCR). In Canada, 31 diagnostic companies applied for the emergency use authorization (EUA) of which 12 are nucleic acid tests and 19 are serological tests (IgM/IgG).
Innovations on diagnostic tools are on-going using different technologies such as new fluorogenic aptamers, nanotechnology, quantum dots, advanced image sensors, electrochemical sensors, microfluidics, and other technologies. Below are some approved diagnostic tools for detecting COVID-19 using proprietary molecular point-of-care test platforms. Most of these diagnostic tools include an assay designed to detect the virus, a microfluidic cartridge, and a reader.

Final thoughts on COVID-19 Medical innovations
The COVID-19 pandemic is a disruptive event in our history. It is a “reset” on the way we live and do things. Even though the current pandemic has had a negative impact on the world, it has given our scientists, engineers and innovators a challenge and motivation to create solutions to the problem. Humans survive because of their creativity, innovations, and ability to create new solutions.
Today, with the technological advancements in computing power, new materials, advanced manufacturing, rapid prototyping, robotics, and state-of-the-art tools and techniques, MedTech innovators can now provide much faster, more efficient, safe and effective solutions to medical conditions today and in the years to come.
Lorenzo Gutierrez is the former StarFish Medical Microfluidics Manager and Interim Toronto Site Director. Lorenzo has extensive experience translating point of care assays to microfluidic cartridges. His microfluidics portfolio includes developing a polyvalence instrument for early infant diagnostics at Chipcare.
Robot Image source: Pexels.com
Read how StarFish Medical led a consortium that created a Ventilator 2.0 therapy device in record time.
