Is there a Theranostic wound dressings market?
Use TPP and B-ASSURED to Design a Novel Medical Device That Meets Market and WHO Needs
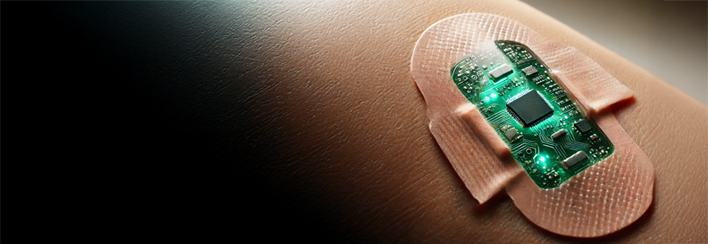
With the recent developments and seemingly ubiquitous nature of real time glucose monitoring and availability of smart wearable tech, the development of a theranostic band-aid seems inevitable. But how practical would this be? Is there a Theranostic wound dressings market? This blog explores theranostic technology and uses target product profile (TPP) and the World Health Organization guidance acronym of B-ASSURED to identify and design a device that addresses the full Theranostic wound dressings market potential.
“Theranostic” is a combination of the words therapeutic and diagnostic, referring to a combined product that can diagnose and provide therapy in the same setting. Theranostic MedTech represents an exciting development in medical technology and personalized medicine. An example in nuclear medicine is the use of radioactive drugs that can identify cancerous tumours and then (combining radionuclide imaging and radiation therapies) to create targeted, more efficient treatment options for certain types of cancer therapies.
Recent developments in artificial intelligence, cell and gene therapies and radio medicine promise great strides in the development of theranostic technology in personalized medicine in the coming years.
An important area of opportunity for theranostic MedTech development is in the development of so-called “Smart Bandages” that can both report on wound healing status or infection and simultaneously delivery therapies (such as anti-inflammatories or antibiotics) in real time as the need may arise.
As a microbiologist I have been working with clients for over 20 years on developing therapies and treatments for one of the most frustrating fields of health care: prevention and management of chronic wounds. This is where theranostic wound dressings may prove their true value.
According to some estimates [1] the global chronic wound care market is projected to grow at a Compound Annual Growth Rate (CAGR) of around 4-7% between 2023 and 2032, reaching a market value of around USD 24 billion by 2032. Given the costs associated with treating and managing chronic wounds and the growth in this area, some of the potential limitations to developing a reasonable theranostic wound dressing (high unit cost, development cost, focused product requirements, and technology limitations) may be addressable in this defined product space.
Target Product Profile (TPP) and B-ASSURED
As a medical device product developer, I work with clients to develop novel devices that can meet a certain target product profile (TPP). Having a well defined and thought out TPP is the hallmark of any product’s probability of eventual success (or failure). For a theranostic wound dressing the critical TPP elements must follow the World Health Organization guidance acronym of B-ASSURED [2].
This guidance is most commonly used in the context of developing infectious disease diagnostics, particularly for those used at the point of care. A theranostic wound dressing must first diagnose the state of the wound and then provide a treatment decision at the point of care. This makes the a B-ASSURED guidance rubric quite appropriate for assessing the market for theranostic wound dressings.
B = Biohazardous.
Consider that the dressing will come in contact with biological fluids and infectious particles and should be treated as biohazardous after/during use. A theranostic system that requires physical contact with a non-disposable reader or expensive, non-disposable electronics would be a potential deal breaker in this use case.
A = Affordable.
Currently wound care has a Cost of Goods Sold (CoGS) target in the range of cents or fractions of a cent. Current standard diagnostic platforms for wound care are typically free (consider traditional and reliable infection indicators of are visual, smell, and heat) and readily and accurately diagnosed by the human eyeball, nose or skin.
To be competitive, theranostic wound care devices in this space must demonstrably provide enhanced performance either through improved time to detection/treatment or outcome. Providing robust economic benefit data tied to health outcomes and reduced health care costs to insurance providers and reimbursement strategies will be a significant challenge for technologies in this space.
S = Sensitive.
An opportunity for theranostic wound care products over the would be provision of an early warning of infection to the patient or the health care provider. The ability to detect a potential infection with greatly increased sensitivity (allowing detection of a few hundred or even individual organisms) would represent a significant improvement over the current state of the art (SOA) baseline and could represent a substantial advantage in the prevention of wounds becoming septic or chronic.
Defining the actual required sensitivity of a wound care product poses a significant challenge in this field. From a microbiology perspective, the skin (and wound environment) provides significant challenges. The skin is not (and should not) be sterile. Developing a dressing that reports bacterial load alone would be challenging in this setting. Single organism level sensitivity would not be a reasonable target for a wound care dressing, but the level of infection, or rate of change would be important markers.
Defining the required detection limit would be impacted by a number of factors (i.e. wound site, age of the wound, severity of the wound, underlying patient conditions) to make meaningful sensitivity tolerances challenging for a simple disposable chemistry-based diagnostic.
S = Specific.
Specificity in theranostic wound care paradigms is a double-edged sword. Consider a wound care dressing that can detect specific pathogens. For example, a wound dressing designed to detect the peptidoglycan in methicillin resistant Staphylococcus aureus (MRSA) would be beneficial for managing treatment options focused on critical organisms of interest and allow commensal (even beneficial) microflora to persist and not trigger a false alarm.
Further, the dressing could release an antibiotic designed to specifically target the MRSA, avoiding the commensals and preventing un-necessary exposure contributing to the problem of antimicrobial resistance build up. On the other hand, this approach might be limited to targeting that potential organism only, which could allow other organisms (like Gram-negatives) to go undetected and untreated.
U = User-Friendly.
Current wound dressing treatments have origins dating back to the dawn of man. Operating within the principles and familiar use case should be considered when designing theranostic dressings. The dressing should be able to fit into the workflow and environment where SOA dressings are found. For example, a theranostic dressing that requires refrigeration or continual charging or power management would not meet most current use cases for SOA dressings.
The diagnostic element of the product further adds complexity to product development. To keep within cost and equipment constraints, a theranostic wound care developer might consider using a colour indicator to signal a change in pH, temperature or presence of other metabolites that indicate a change in wound state. The colour indicator would need to be distinguishable and user-friendly (e.g. a wound dressing with a difficult colour to interpret).
R = Rapid/Robust.
A standout advantage to theranostic wound care is that typical wound care provides sufficent time for theranostic diagnosis and treatment. Dressings are typically worn for extended periods of time allowing for diagnostics to develop. Dressing changing frequencies (daily to every three days) allows for opportunities for built-in chemistry reset or calibration. This extended exposure provides a unique opportunity for therapy delivery to be released over time or in response to physiological changes (i.e. pH, temperature, metabolic response etc.).
Utilizing a simple chemistry-based approach to diagnostics or therapy delivery may limit the dressing’s robustness in terms of adapting to changes in wound state over time (e.g. once the therapy is released the opportunity for dynamic control may not be available). However, the disposable nature of wound care dressingscould enable replenishing with fresh indicators and therapy during each dressing change.
E = Equipment Free.
A theranostic wound care dressing that incorporates the diagnostic and the therapy in a simple equipment-free form factor would have tremendous advantages. Indeed, many developers in this space are focused on chemistry-based diagnostics (i.e. colour change in response to changes in wound state/infection) and chemistry-based release of therapy (i.e. release of a drug in response to metabolism/changes in healing processes) thus satisfying the equipment-free requirement.
Recent advances in micro-electronics and electronic communications hardware have led to an explosion in technologies, platforms and products enabling real-time monitoring and drug delivery in the diabetes space. Extending these advances to the field of wound care would provide tantalizing opportunities for theranostic wound care developers. Given the rubric’s scoring for equipment free options, the lure of more complicated delivery and monitoring systems should be considered carefully in this specific TPP (i.e. cost will be the most significant driver).
D = Deliverable & Disposable.
Wound care dressings, by the nature of their application, should consider the use case environment where the dressing is able to be rapidly and efficiently deployed, worn for an acute period, and then safely disposed. Investing in a theranostic wound care dressing that can precisely monitor and report in real time on wound and infection state while dynamically delivering therapies over the expected lifespan of the device autonomously is a noble goal. However, the reality of the use case environment, cost, acute use, and the disposable nature inherent in wound dressings must be considered and underscore the decisions made along the product development journey.
Theranostic Wound Dressings Market Conclusions
When considering TPP in general, the key element that any product should have is a clear competitive advantage over similar products. In theranostic wound care, this is the ability to Diagnose and Treat. Clearly, this ability is a standout in the field of general wound care.
However, from the application of the B-ASSURED rubric to a potential theranostic wound dressing for general use, it is clear that there are some large technical hurdles yet to be overcome. Most importantly, the grand challenge for a theranostic wound care product will be delivering this key feature in a form factor and (more importantly) price point that will be adoptable by the market. For general ‘every day’ applications, it is unlikely that a theranostic dressing would be a viable option.
Not all wound care applications are the same. Our team of biomedical experts welcome the opportunity to help your team understand and develop innovative medical device projects like the theranostic wound care product discussed in this article.
[1] https://www.fortunebusinessinsights.com/industry-reports/chronic-wound-care-market-100222
[2] WHO actually only suggests the “ASSURED” acronym, I added the “B” and put it first because the consideration of Biohazard containment should be top of mind when developing products in this space.
Nick Allan is the Bio Services Manager at StarFish Medical. He has provided innovative solutions to client issues ranging from proof-of-concept studies for rapid detection point of care assays to full scale regulatory submission studies, and designed and facilitated more than 500 Unique Research Protocols.
Images: AI-generated image
Key success factors in designing, developing wearable medical devices plus the importance of selecting appropriate adhesives.
Related Resources

A structured, well-documented design review process is a critical component of successful product development, particularly in the medical device industry.

In medical device development, we deal with complex projects that span multiple disciplines, timelines, and regulatory gates. It’s a constant balance between moving fast enough to innovate, but slow enough to stay compliant.
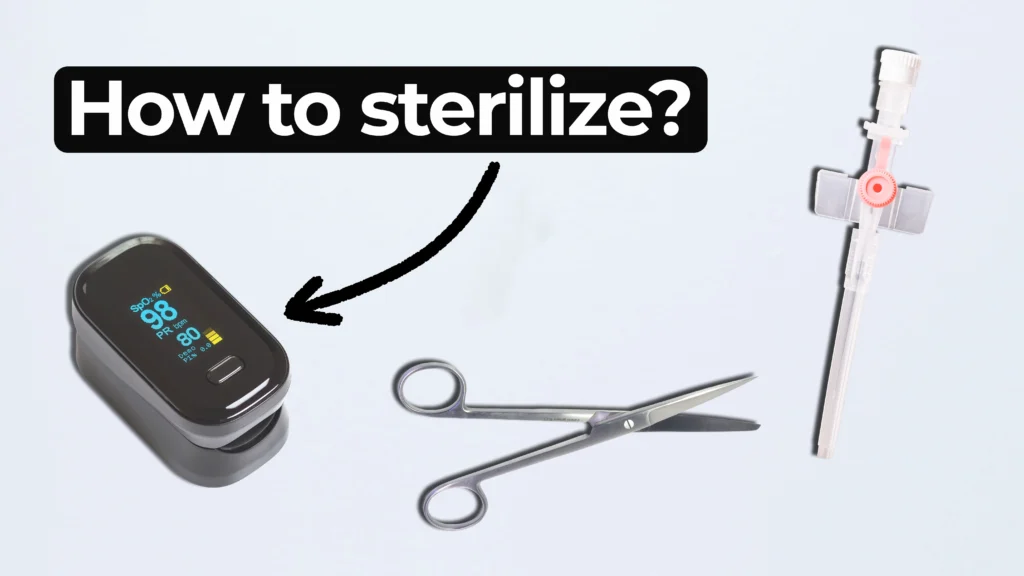
Ariana and Mark walk through FDA-approved options and explain how to select the right one for your product. From metals to plastics and electronics, not all devices can handle the same process.
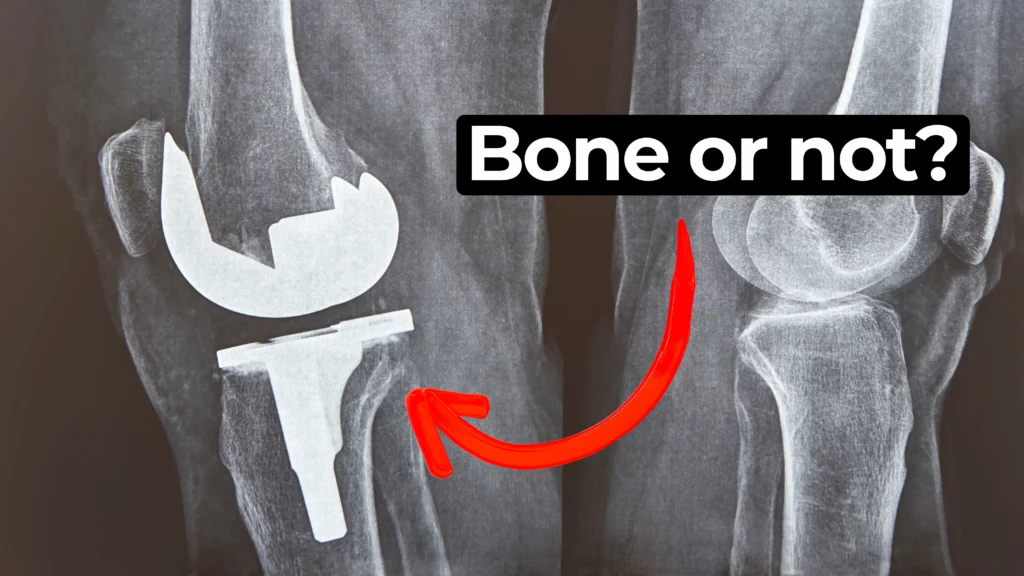
In this episode of MedDevice by Design, Ariana and Mark dive into the biomechanics and materials science behind osseointegration for implants.