Puff the Magic Tonometer Workflow
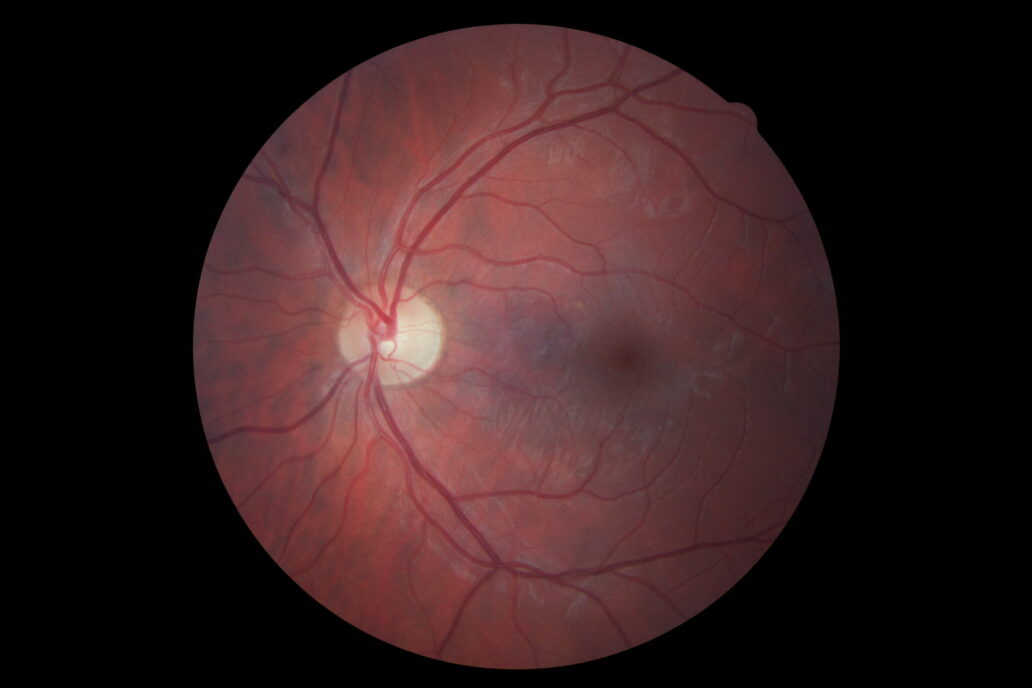
This is a picture of the back of my eye from a recent visit to my friendly ophthalmologist. I’m told everything is relatively healthy and that my mild astigmatism will not get worse as my eyes trend down the path of presbyopia… but that’s not why I am writing this. In stepping through the various tests, I couldn’t help to feel a little eye violated when the tonometer sent a puff of air into my eye – and it sparked my interest.
Ophthalmologists and patients alike are familiar with this non-contact Tonometer measurement to determine the intraocular pressure (IOP) in order for doctors to gain insight to potential glaucoma and a variety of other indications.
I discussed the history of the Tonometer device with our President, Scott Phillips and I found it interesting that the tonometer’s evolution to the masses started off as a contact instrument (such as Goldmann) that physically contacted the cornea and ‘progressed’ to less accurate and more complicated non-contact tonometry.
Why replace an accurate test with a more complicated and less accurate one? Simple. Because now less trained operators can use it. In my recent visit, the ophthalmologist was left with more time to analyze results and discuss them with me, while a trained technician was able to perform the mundane (and in this case mildly annoying) tasks.
Subsequent iterations of the tonometer have refined it’s abilities to better quantify the intraocular pressure, but it exemplifies the benefit of understanding the workflow, potential users, and the impacts of CLIA in assessing core technology options.
Mark Drlik is a Concept Development Manager at StarFish Medical. He uses Quality Function Deployment (QFD) and gut feel to design medical devices.
Image: StarFish Medical