Osseointegration Implants: How They Work and Why They Matter
In this episode of MedDevice by Design, Ariana and Mark explore the science behind osseointegration implants. These devices support bone growth directly onto the implant surface, improving stability for joint replacements, dental prosthetics, and even load-bearing limb implants.
What Are Osseointegration Implants?
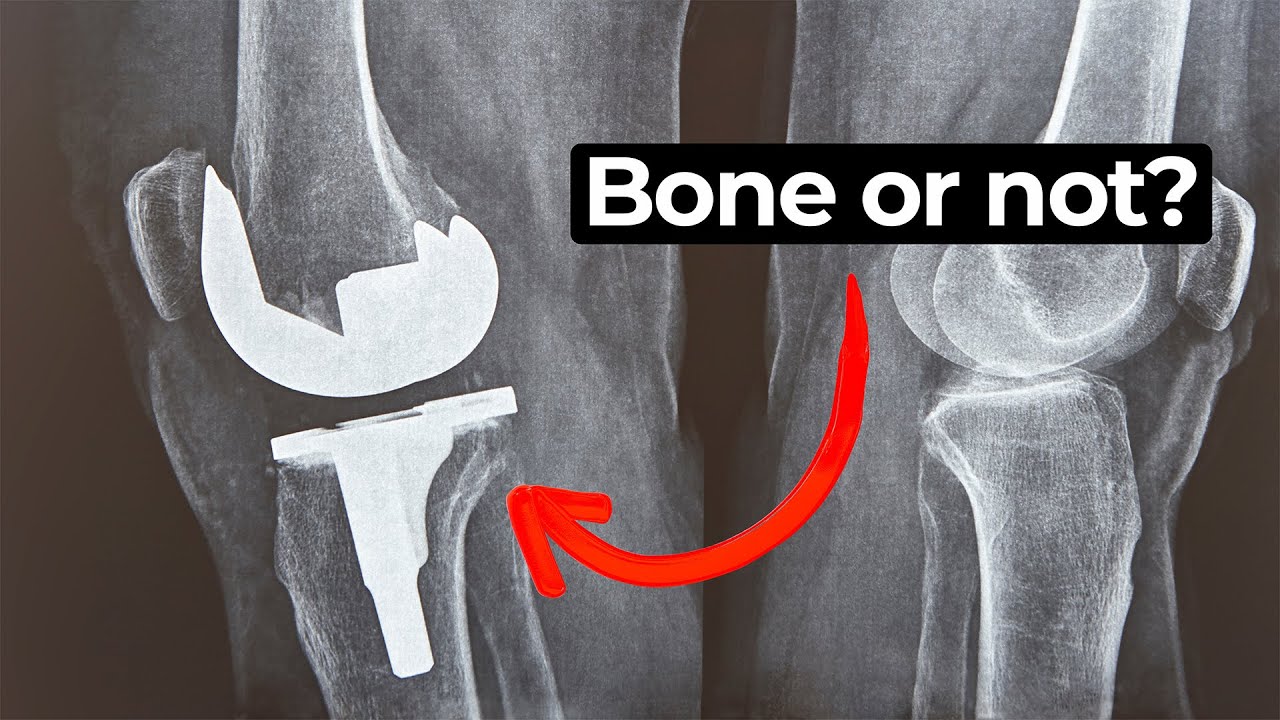
Osseointegration refers to the process by which bone cells grow and attach directly to an implant. For medical devices like hip or knee replacements, this connection helps create a secure fit between the bone and the device. Ariana explains that successful integration is critical for the long-term success of implants.
Surface Design for Bone-Integrated Implants
Mark and Ariana discuss the importance of surface coatings and structure. Materials like titanium are commonly used for their biocompatibility, and coatings such as hydroxyapatite help trigger a positive osteogenic response. The implant’s surface texture also plays a vital role. Micro- and nano-scale features encourage protein and cell adhesion, while larger pores support vascularization.
The Role of Motion in Implant Integration
Interestingly, not all movement is bad. Mark notes that a small amount of micromotion—between 50 and 150 microns—can actually encourage bone growth. However, movement beyond that threshold may lead to fibrous tissue development instead of strong bone attachment, ultimately weakening the implant over time.
A Delicate Balance in Design
Designing for osseointegration implants means striking a careful balance. The material, surface finish, and even the mechanical loading of the implant all need to work together to achieve optimal results. Ariana and Mark highlight how precision engineering at every level of the device contributes to successful long-term outcomes.
Enjoying MedDevice by Design? Sign up to get new episodes sent to your inbox.
Related Resources

Nick and Nigel walk through how sterile disposables are processed and verified before they reach the field.
The FDA agentic AI is making headlines after the agency announced its own internal AI review tool. In this episode of MedDevice by Design, Ariana and Mark discuss what this could mean for medical device submissions and regulatory efficiency.

The sandwich ELISA assay is one of the most common ELISA formats used in diagnostics. Nick and Nigel walk through the method step by step using simple visuals and plain language.